A recent video presentation by Prof Ivor Mueller, Walter and Eliza Hall Institute of Medical Research (WEHI), Melbourne, reveals progress in the fight to eliminate asymptomatic P. vivax. Thanks to RAM District Supervisor Shelley Gurney (D9810) for bringing the video to our attention. The presentation was useful as it takes our understanding one step further from what we learned from Prof Shanks at the 2020 Virtual Conference.
Some key points:
- P. vivax is harder to eliminate because the majority of patients can be infectious but current diagnostic tools cannot pick up these asymptotic and low-density infections (submicroscopic) in the blood. And, ~50 to 80% of relapses in pre-school and primary school children are caused by hypnozoites reservoir (sleeping parasites) in the liver. Treating only those clinically positive P. vivax will mean that we miss a majority of malaria positive cases.
- Importantly, “Elimination will be slow without directly attacking the ‘hidden’ hypnozoite reservoir (in the liver).” (Prof Ivor Mueller, 2018).
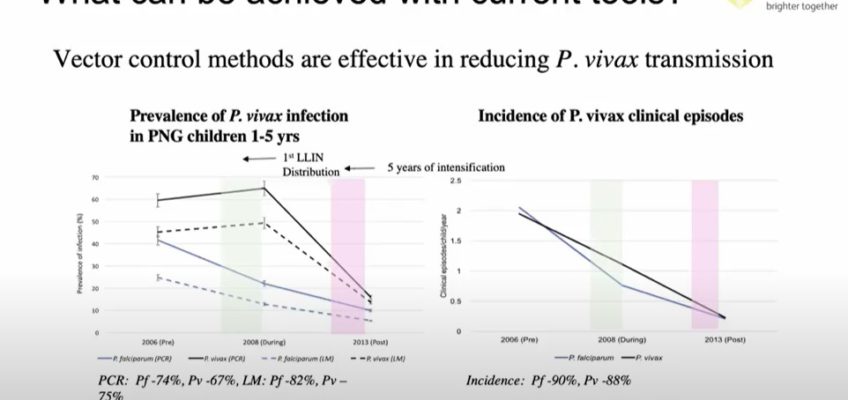
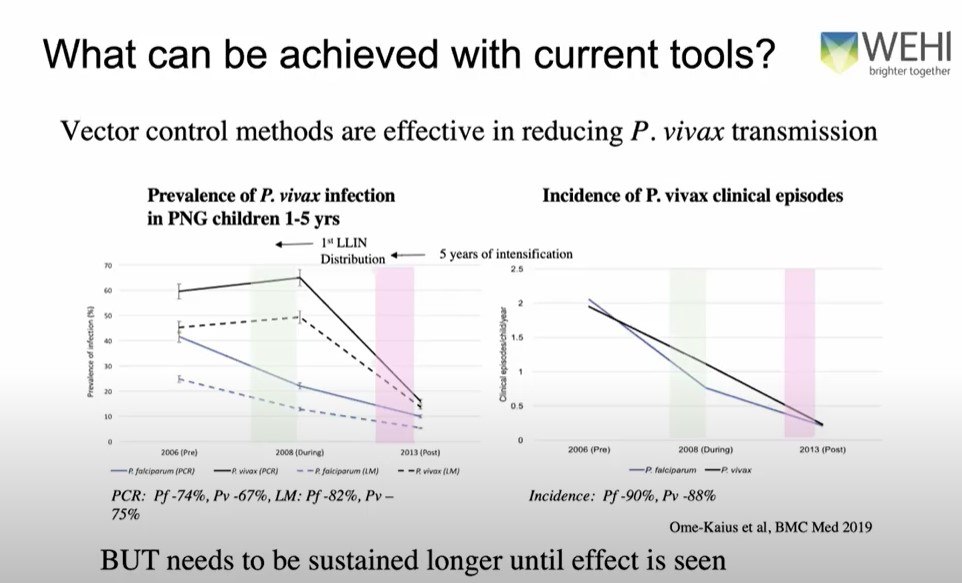
- Research in PNG shows that universal access to bed nets are effective to reduce malaria but we need to maintain use for a longer time (eg 5 years) and this could be because of the reservoir of ‘sleeping parasites’. Cases were reduced by ~88% in 5 years.
- And a new tool – the new antibodies testing method is encouraging! It can detect 80% of antibodies in patients infected between one (1) to 9 months. Thus, treating those with antibodies may prevent replacing infections.
Relevance to RAM:
- Bed nets are effective in our region (even when there is insecticide resistance).
- We’re hoping to support the use of malaria risks stratification training in West Timor, NTT Province, Indonesia, so, good to hear others are also applying this stratification process.
- In the Central Province, Solomon Islands, in 2014, where there were 12% of 1,000 children infected, a majority of cases were mostly P. vivax and only 0.3% P. falciparum. The new project that RAM is planning in the Solomon Islands may therefore need to support the use of G6PD point of care testing and Primaquine use.